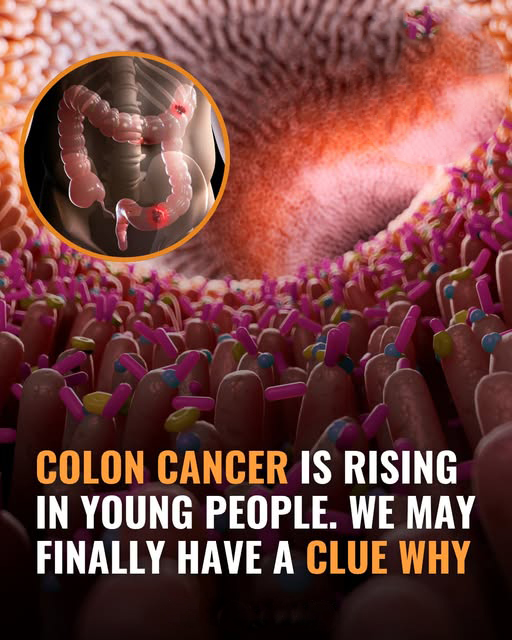
In recent years, medical professionals and researchers have been sounding the alarm over an unsettling trend—colon cancer is increasingly affecting younger adults, many of whom are under the age of 50. Once considered a disease primarily associated with older populations, colorectal cancer is now appearing more frequently in people in their 20s, 30s, and early 40s. This shift has puzzled the medical community and raised urgent questions about what might be driving this surge.
For decades, routine colon cancer screenings typically began around the age of 50, based on the assumption that younger individuals were not at high risk. But that assumption is being rapidly challenged by new statistics and real-life cases. More and more young adults are being diagnosed with advanced stages of the disease, often without having experienced clear warning signs or having any known family history of cancer.
So what could be behind this sudden rise?
Experts have been examining a variety of possible contributing factors, and while no single explanation has been confirmed as the sole cause, a combination of lifestyle, dietary habits, environmental exposure, and biological changes seems to be involved. One of the major points of concern is the modern diet. The prevalence of ultra-processed foods, red meats, sugary beverages, and low-fiber diets may be playing a significant role in disrupting gut health and increasing inflammation in the digestive system. These dietary patterns are especially common among younger demographics, who may rely more heavily on fast food and convenience meals.
Another potential contributor is the sedentary lifestyle that has become common in the digital age. Long hours spent sitting at desks, working on computers, or scrolling through smartphones can reduce physical activity levels, which are known to impact overall digestive health and immune system function. Combined with stress, poor sleep, and irregular eating schedules, these habits may set the stage for internal imbalances that lead to chronic disease.
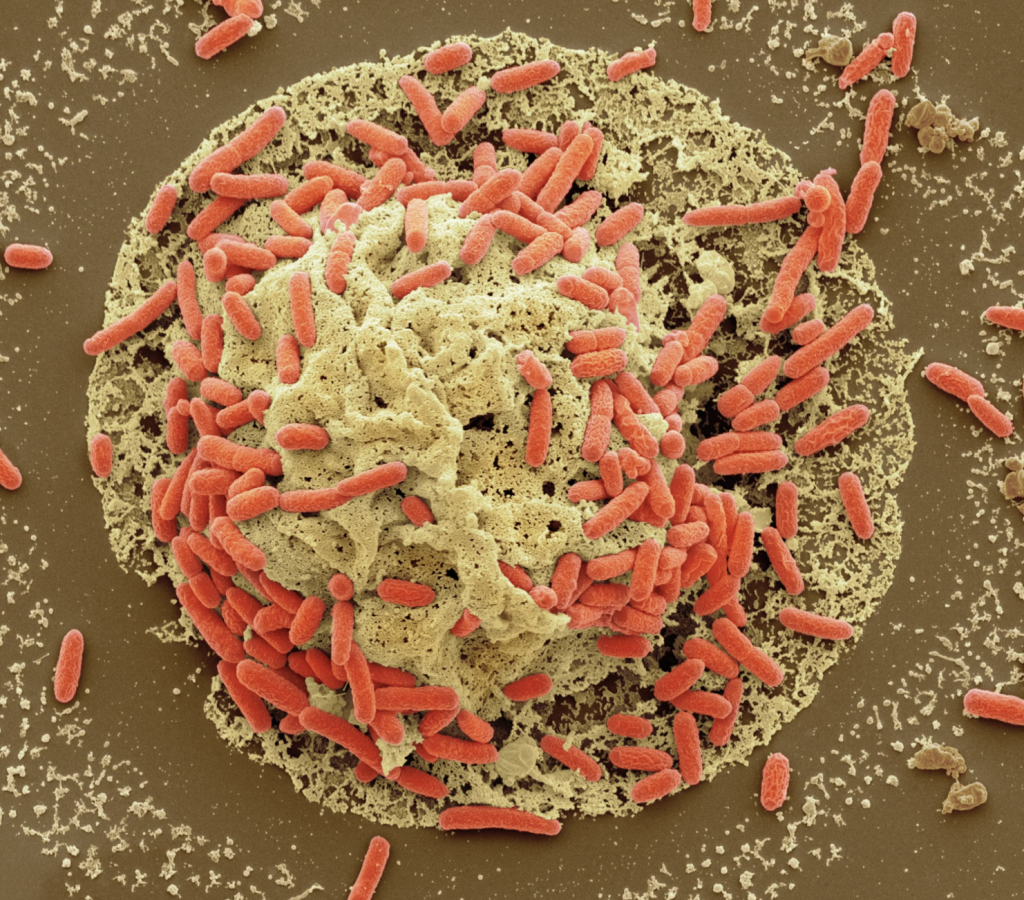
There’s also growing interest in how changes to the gut microbiome—the trillions of bacteria living in our intestines—might influence the development of colorectal cancer. Emerging research suggests that an unhealthy microbiome can increase inflammation and disrupt normal cell processes in the colon, potentially contributing to the growth of cancerous cells.
What makes this trend even more alarming is that many young adults are often misdiagnosed or diagnosed late. Because colon cancer has traditionally been associated with older age groups, many early warning symptoms—such as fatigue, unexplained weight loss, abdominal discomfort, or changes in bowel habits—are often overlooked or attributed to more common conditions like stress or irritable bowel syndrome. This delay in diagnosis means that many young patients are only identified once the disease has reached an advanced stage, making treatment more difficult and outcomes less favorable.
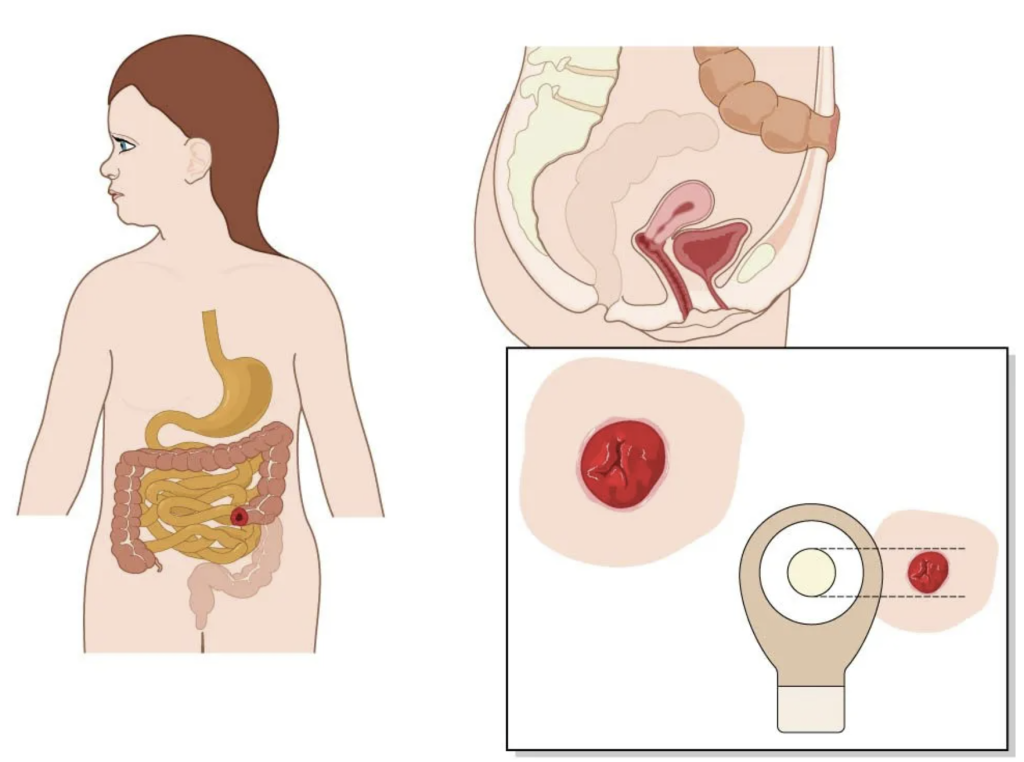
In response to the growing number of cases, some health organizations have already lowered the recommended age for routine colon cancer screenings. However, awareness remains low, and many young adults do not consider themselves at risk. Educating the public, especially younger generations, about the symptoms and risk factors of colon cancer is crucial in promoting early detection and improving survival rates.
Ultimately, the rising incidence of colorectal cancer in young adults is not just a medical mystery—it is a public health warning. It calls for increased vigilance, better awareness, and a collective reevaluation of lifestyle choices. While researchers continue to search for definitive answers, the trend itself is a clear signal: colon cancer is no longer a disease of old age, and the younger generation must begin taking proactive steps for their long-term health.