Chronic Venous Insufficiency (CVI) has become a topic of public interest recently after former President Donald Trump reportedly received this diagnosis. To shed light on the condition and its implications, here’s a comprehensive breakdown of CVI, its symptoms, risk factors, management strategies, and how it may relate to everyday life—all explained clearly and informatively.
What Is Chronic Venous Insufficiency?
Chronic Venous Insufficiency occurs when the veins in the legs are unable to pump blood efficiently back to the heart. Under normal circumstances, valves inside veins open to let blood flow upward and close to prevent backflow. In CVI, these valves malfunction or become damaged, causing blood to pool in the lower extremities. Over time, this leads to symptoms such as swelling, pain, skin discoloration, and in severe cases, open sores (ulcers).
People with CVI often experience:

- Swollen ankles or calves: Often worse after standing or sitting for long periods
- Aching, heavy legs: Particularly after activity
- Varicose veins: Enlarged or twisted veins visible under the skin
- Itchy, dry, or discolored skin: Over time, blood pooling can cause brownish discoloration
- Leg cramps or restless legs: Especially at night
- Venous ulcers: Painful sores that resist healing and may recur
These symptoms can range from mild discomfort to debilitating pain and mobility issues, depending on the severity of venous damage.
A variety of factors can increase one’s likelihood of developing CVI, including:
- Age: Symptoms often appear after age 50
- Family history: Genetics play a strong role
- Obesity: Excess weight places added pressure on leg veins
- Prolonged standing or sitting: Jobs that involve long periods of immobility elevate risk
- Pregnancy: Increased blood volume and pressure on veins can contribute
- Blood clots or leg injury: Prior DVT (deep vein thrombosis) or trauma can damage valves
In the case of anyone, including public figures, multiple risk factors can converge over time, gradually weakening vein valve function.
When chronic venous insufficiency is suspected, doctors perform a thorough assessment that may include:
- Physical exam: Checking legs for swelling, varicose veins, and skin changes
- Patient history: Evaluating symptoms and lifestyle risk factors
- Duplex ultrasound: A primary diagnostic tool that uses sound waves to show blood flow and detect valve leakage or obstructions
Additional imaging tests may be used in complex cases to assess deeper veins or rule out other circulatory issues.
While CVI is generally a long-term condition, various strategies can help manage symptoms, prevent progression, and improve quality of life:
Compression therapy:
Graduated compression stockings remain the first-line non-invasive option. They help reduce swelling and improve circulation by applying gentle but firm pressure.
Lifestyle adjustments:
Losing weight, exercising, avoiding prolonged sitting or standing, and elevating the legs above heart level regularly can significantly alleviate discomfort and slow disease progression.
Medical procedures:
For more advanced cases, minimally invasive procedures include sclerotherapy (injecting chemical agents to close small veins), endovenous laser therapy (EVLT), or radiofrequency ablation (RFA), which use heat to seal problematic veins.
In rare and severe cases, surgical vein stripping or bypass grafts may be considered.
Skin care and ulcer management:
Proper hygiene, moisturizing, and dressing changes help heal skin irritation and prevent infection. In cases of ulcers, wound care specialists may use specialized dressings or even advanced therapies like skin grafts.
Living With CVI: Practical Guidelines
- Daily compression stockings: Choose proper fit and wear consistently. Don’t skip days—uninterrupted wear yields best results.
- Movement breaks: Even gentle walking or stretching at intervals can help.
- Leg elevation: Aim for 3–4 times per day, each session lasting about 15–20 minutes.
- Weight control: A balanced diet and regular exercise reinforce vein health.
- Footwear: Comfortable shoes without tight straps benefit venous return.
- Regular follow-up: Venous insufficiency can progress if left unchecked, so routine check‑ups help catch complications early.
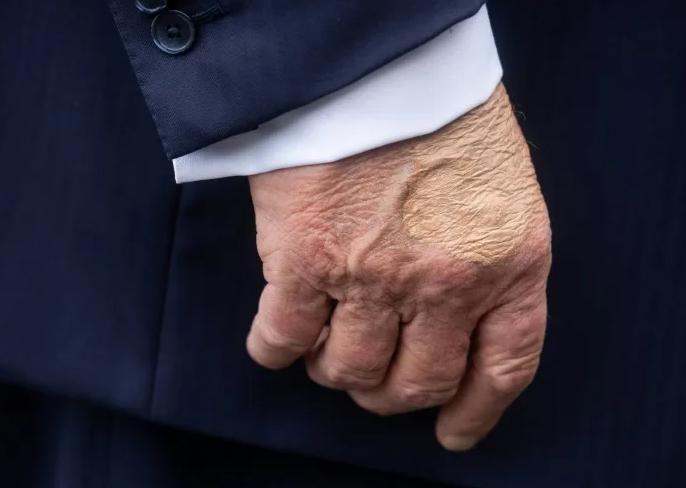
What It Means for Public Figures Like Trump
High-profile leaders, such as former Presidents, often undergo frequent medical exams, which may uncover chronic conditions like CVI. Fortunately, CVI is manageable, and with lifestyle modifications and possible procedures, it typically does not interfere with daily functioning—even at the demanding pace of a public figure’s schedule.
Treatment offers two-fold benefits: it eases physical symptoms (like swelling or discomfort during travel) and can mitigate future risks, such as the development of ulcers or blood clots.
Chronic Venous Insufficiency is a common but manageable circulatory condition. While it won’t go away, with diligent care and treatment, individuals can maintain comfort and mobility. For anyone diagnosed—public figure or private individual—the combination of medical treatments, lifestyle adjustments, and routine monitoring offers a roadmap to living well with CVI. Ultimately, understanding the condition helps remove stigma and emphasizes that proper care can allow people to continue their daily activities with minimal disruption.