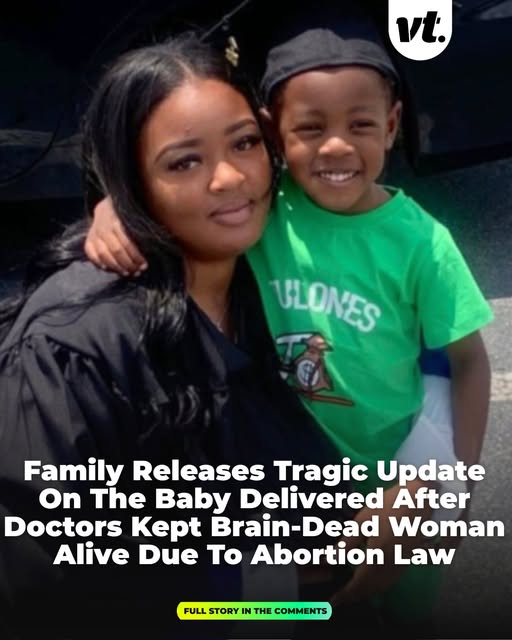
In a heartbreaking and controversial case from Georgia, a pregnant woman was declared brain‑dead, yet kept alive on life support so her unborn child could be delivered. The woman, a nurse, had been around eight to nine weeks pregnant when she suffered deadly brain clots. After being pronounced brain-dead, doctors maintained life support not for the mother’s benefit, but to allow her fetus to continue developing under state law.
Nearly four months later, on June 13, the baby boy was delivered via emergency cesarean section at a hospital. The newborn, named Chance, was born prematurely and weighed only 1 pound, 13 ounces (about 538 grams). Following the delivery, the mother was removed from life support. The dramatic circumstances immediately drew national and international attention, sparking deep ethical, legal, and human rights debates.
Why She Was Kept Alive
The decision to keep the woman alive came down to legislation in her state. Georgia enforces a so‑called “heartbeat” law: after fetal cardiac activity is detected — usually around six weeks into pregnancy — abortion is effectively banned. Because her fetus had a detectable heartbeat, hospital officials said they were compelled to keep her body functioning until the baby could survive outside the womb. Her family was reportedly denied the right to make decisions about life support discontinuation. For her relatives, this felt like torture. They watched as their loved one lay motionless on machines, knowing she was legally dead — yet unable to end life support because the law prioritized fetal rights over the family’s wishes.

Difficult Delivery and Fragile New Life
When the baby was born, he faced a precarious start. Born significantly premature, he was immediately admitted to neonatal intensive care. His birth weight placed him in the extremely vulnerable preemie category, and medical staff were cautious about his chances. Family members expressed concern that he might face serious long-term health problems, including potential vision issues, neurological impairment, or mobility limitations. Despite the grim outlook, there was cautious hope. His grandmother said that “he’s expected to be OK. He’s just fighting,” and asked for prayers for his survival. The newborn’s critical condition underscored both the fragility of premature life and the emotional weight carried by his family as they awaited news.
Ethical and Legal Fallout
This case reignited heated debate about medical ethics, reproductive rights, and state versus family control over life decisions. Many view it as a disturbing example of what can happen when laws designed to protect unborn fetuses override the autonomy and rights of women and families. Critics argue that no one should be forced into such a prolonged and traumatic state — legally dead, yet artificially kept alive — simply because of their pregnancy. Supporters of fetal protection laws see the case differently, arguing for the preservation of life wherever possible. Still, the complexity of a brain-dead woman being kept alive solely for fetal viability raises urgent questions about consent, dignity, and the boundaries of medical decision‑making.
The Family’s Struggle and Hope
For the woman’s family, the emotional toll has been enormous. They lost a daughter and mother — yet also hold onto a glimmer of hope for her newborn son. The grandmother, speaking publicly, said the family loved the idea of saving the baby, but believed they should have had a say. “She’s pregnant with my grandson,” she said, “but that grandson may be blind, may not walk. We don’t know if he’ll survive.” As the newborn fights for survival in intensive care, relatives and supporters have rallied behind the family, offering emotional support and raising funds for medical expenses. The case has also inspired public outcry and demands for legal review — many urge lawmakers and medical providers to reconsider how such tragic circumstances are handled in the future.

A Complex Legacy
This story highlights the painful human consequences when legal frameworks, medical decisions, and deeply personal tragedies collide. On one hand, a premature baby named Chance got a chance at life. On the other, the mother’s death — and the family’s heartbreak — underline the heavy cost of enforcing laws without flexibility or consent. It remains to be seen what physical and emotional journey awaits the newborn, and whether legal reforms will follow. But for now, this case stands as a haunting example of how advances in medicine and changing laws can lead to morally fraught, deeply human dilemmas.