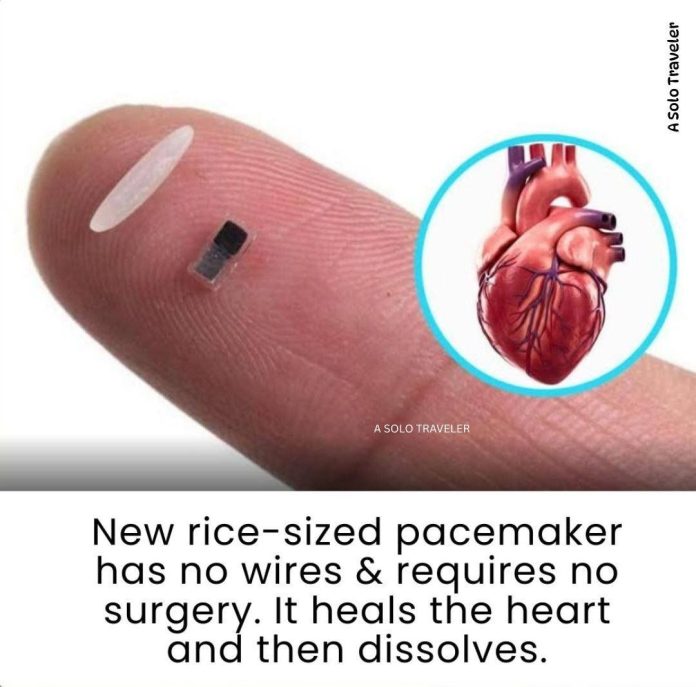
Imagine a device so small that it fits inside a syringe, yet powerful enough to regulate a heartbeat—and then simply dissolves when its job is done. What once sounded like science fiction is now becoming reality, thanks to a remarkable advancement in medical technology: the development of a rice‑sized, dissolvable pacemaker.
From Burden to Breakthrough
Traditional temporary pacemakers have long been critical in post-operative cardiac care. Whether implanted temporarily after congenital heart defect surgeries in newborns or following adult open-heart procedures, these devices rely on bulky electronics and leads that pierce the chest and tether patients to external power sources. Eventually, removal requires another invasive procedure—often risking infection, bleeding, or even damage to the heart muscle via scar tissue adhesion.
Tragic historical cases, like that of astronaut Neil Armstrong, who suffered internal bleeding following the removal of such a pacemaker in 2012, highlight the potential dangers.
The need for a safer, less invasive solution became obvious.
Redefining the Implant: A Tiny, Dissolvable Device
Engineers at Northwestern University, led by Professor John A. Rogers and cardiologist Igor Efimov, took on the challenge. Their vision? A wireless pacemaker less than a grain of rice in size, built entirely from biocompatible and bioresorbable materials that naturally dissolve after fulfilling their purpose.
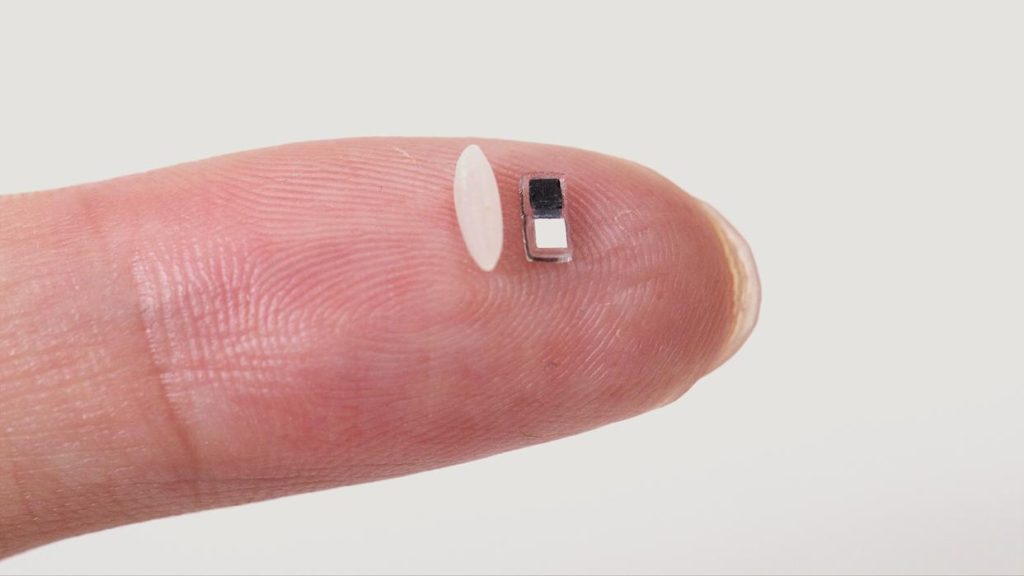
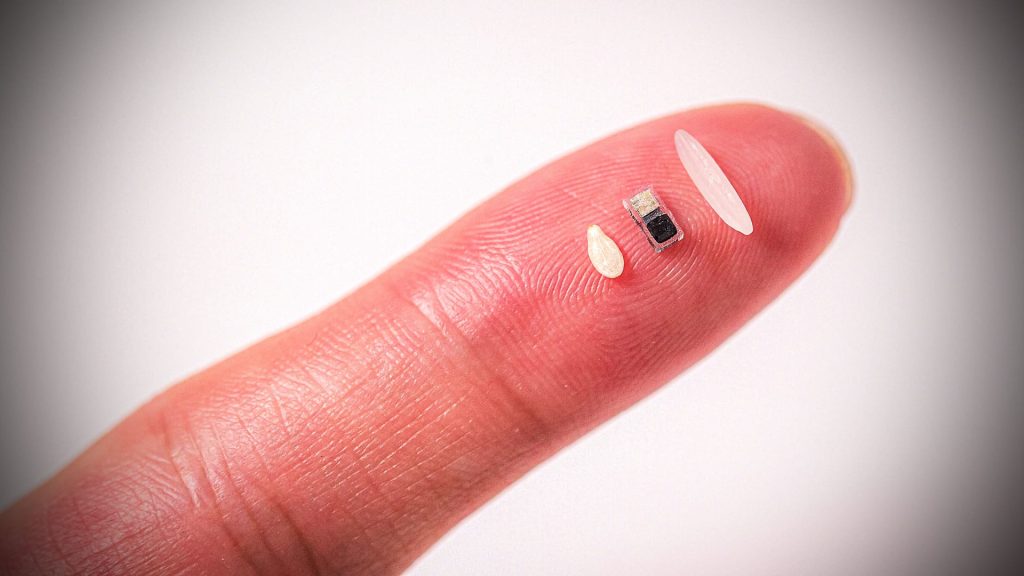
Measuring approximately 1.8 mm × 3.5 mm × 1 mm, the device can be injected via syringe onto the heart during surgery—no incisions, wires, or secondary extraction needed.
Engineering Simplicity: How It Works
Despite its size, the pacemaker delivers fully functional cardiac pacing:
- Power source
Instead of batteries, it uses a galvanic cell—two metal electrodes that create electrical current when bathed in the body’s fluids, acting as a natural electrolyte - Wireless control
A gentle, infrared LED pulse is emitted from a soft wearable patch on the chest. Infrared light penetrates skin, muscle, and bone to reach the pacemaker and switch it on - Heartbeat sensing & pacing
The patch monitors cardiac rhythm. When an irregular heartbeat is detected, it flashes light pulses that trigger the pacemaker to respond by sending targeted electrical stimulation—maintaining a steady beat - Self-dissolving
After roughly one week, when hearts of newborns typically recover from congenital surgery, the pacemaker’s materials degrade and are naturally reabsorbed—eliminating the need for risky removal procedures - Clinical Promise and Pediatric Potential
The prime motivation behind this innovation is helping infants. Roughly 1% of babies worldwide are born with congenital heart defects, often requiring temporary pacing after corrective surgery.
The window of about seven critical days post-operation demands stable pacing—but conventional temporary pacemakers pose significant risks during implantation and removal.
This tiny, dissolvable device is tailored to alleviate those risks. By enabling less invasive placement, minimal post-op trauma, and no secondary surgery, it offers a gentler, safer path to recovery
While newborns are the primary focus, its advantages extend to adult cardiac care too—patients recovering from bypass surgery, valve replacements, or trauma could benefit from a temporary pacemaker that self-resorbs without requiring device management.
Expanding the Scope: Beyond Pacemakers
This innovation marks a milestone in bioelectronic medicine. The same platform technology—microscopic, wireless, and dissolvable devices—can be adapted for:
- Multisite heart pacing using different light wavelengths, enabling complex cardiac synchronization.
- Integration with heart valves or other implants to support tissue function during early healing.
- Broader therapeutic uses, such as promoting nerve regrowth, fostering bone recovery, aiding wound healing, or even localized pain control.
Professor Rogers describes it as a paradigm shift: devices that heal the body, then dissolve—offering safe and precise therapy tailored to each patient’s journey.
Path to Human Use & Future Outlook
Prototypes have delivered successful results in animal models—from rodents to pigs—and have demonstrated efficacy on human donor hearts in lab conditions. Human clinical trials may begin in two to three years, as the FDA reviews submissions from the research team.
Looking ahead, we stand on the brink of a new era in minimally invasive cardiac interventions, supported by customizable, biodegradable electronics that vanish when their job is done.
A Future Where Healing Leaves No Trace
This rice‑sized marvel is proof that the future of medicine lies in subtlety and harmony with the human body. It promises less trauma, fewer complications, and more compassionate care—especially for our most fragile patients.
Rather than adding foreign hardware into vulnerable hearts, we now have tools that support, adapt, and disappear. This tiny pacemaker heralds a future of healing that respects the body’s natural integrity—and invites us to reimagine what it means to care for the human heart.