Psoriasis is a chronic autoimmune skin condition that affects millions of people worldwide. It manifests in various forms, each with distinct characteristics and symptoms. Recognizing the early signs of psoriasis is crucial for effective management and treatment. This article delves into the key symptoms, types, causes, and treatment options for psoriasis, aiming to provide a comprehensive understanding of the condition.
Understanding Psoriasis
Psoriasis is an immune-mediated disorder where the immune system mistakenly attacks healthy skin cells, leading to rapid skin cell turnover. This accelerated process results in the accumulation of skin cells on the surface, forming thick, scaly patches that can be itchy, painful, and sometimes crack or bleed. While the exact cause remains unknown, a combination of genetic predisposition and environmental triggers is believed to contribute to its development. Common triggers include infections, stress, certain medications, and injuries to the skin.
Five Warning Signs of Psoriasis

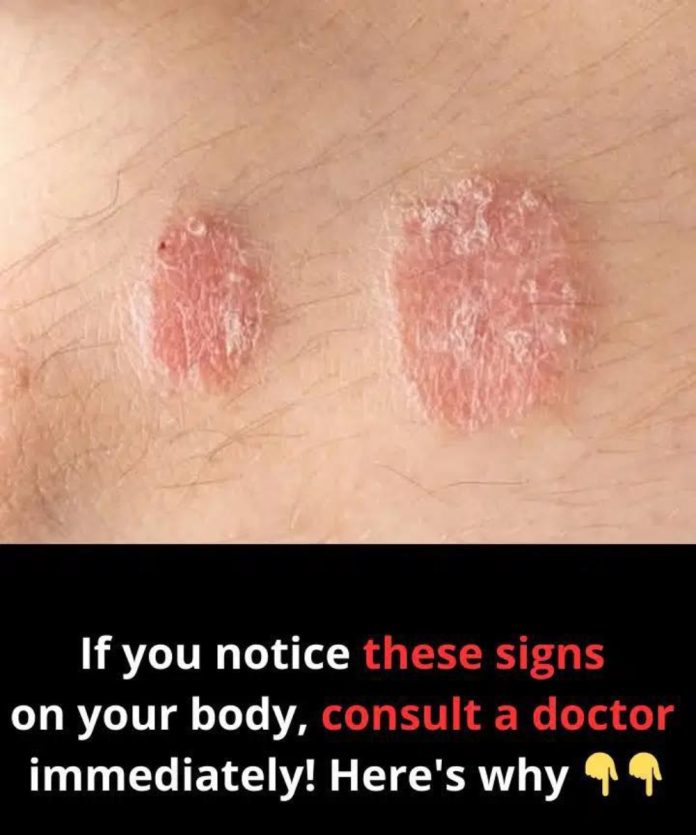
Red, Inflamed Patches of Skin
One of the hallmark signs of psoriasis is the appearance of red or pink patches of inflamed skin, often covered with silvery-white scales. These patches, known as plaques, commonly occur on the elbows, knees, scalp, and lower back. They can be itchy and may crack or bleed if irritated.
Dry, Cracked Skin That May Bleed
Psoriatic lesions often lead to extremely dry skin that can crack and bleed. This symptom not only causes discomfort but also increases the risk of infection. Moisturizing regularly can help manage this symptom, but persistent cracking and bleeding warrant medical attention.
Itching, Burning, or Soreness
Affected areas may experience sensations of itching, burning, or soreness. These sensations can range from mild to severe and may interfere with daily activities and sleep. Scratching can exacerbate the condition, leading to further skin damage.
Thickened or Ridged Nails
Psoriasis can affect the nails, leading to pitting (small dents), abnormal nail growth, discoloration, and separation of the nail from the nail bed (onycholysis). These changes can be both cosmetic and functional, sometimes causing discomfort or difficulty in performing tasks.
Stiff and Swollen Joints
In some cases, psoriasis is associated with psoriatic arthritis, which causes joint pain, stiffness, and swelling. This condition can affect any joint and may lead to permanent joint damage if not treated promptly. Early diagnosis and intervention are crucial to prevent long-term complications.
Types of Psoriasis
Understanding the different types of psoriasis is essential for accurate diagnosis and treatment:
- Plaque Psoriasis: The most common form, characterized by raised, inflamed patches covered with silvery-white scales.
- Guttate Psoriasis: Often triggered by bacterial infections like strep throat, it presents as small, drop-shaped lesions primarily on the trunk and limbs.
- Inverse Psoriasis: Appears as bright red, shiny lesions in skin folds, such as under the breasts, around the groin, or in the armpits.
- Pustular Psoriasis: Characterized by white pustules (blisters of noninfectious pus) surrounded by red skin, commonly occurring on the hands and feet.
- Erythrodermic Psoriasis: A severe, potentially life-threatening form that leads to widespread redness, severe itching, pain, and skin shedding. It requires immediate medical attention.
Causes and Triggers
While the exact cause of psoriasis is not fully understood, several factors are known to contribute to its onset and flare-ups:

- Genetic Predisposition: Having a family history of psoriasis increases the risk of developing the condition.
- Immune System Dysfunction: An overactive immune system attacks healthy skin cells, accelerating skin cell production.
- Environmental Triggers: Infections, skin injuries, stress, smoking, and certain medications (like lithium and beta-blockers) can trigger or exacerbate psoriasis symptoms.
Treatment Options
While there is no cure for psoriasis, various treatments can help manage symptoms and improve quality of life:
- Topical Treatments: Corticosteroids, vitamin D analogs, and moisturizers are commonly used to reduce inflammation and scaling.
- Phototherapy: Controlled exposure to ultraviolet (UV) light can slow skin cell turnover and reduce scaling and inflammation.
- Systemic Medications: For moderate to severe cases, oral or injectable medications like methotrexate, cyclosporine, or biologics may be prescribed to target specific parts of the immune system.
- Lifestyle Modifications: Maintaining a healthy weight, managing stress, avoiding known triggers, and adhering to a skincare routine can help control symptoms.
When to Seek Medical Advice
If you notice persistent skin changes, such as red patches, scaling, or nail abnormalities, it’s essential to consult a healthcare provider. Early diagnosis and treatment can prevent complications, including joint damage from psoriatic arthritis. A dermatologist can provide a tailored treatment plan based on the type and severity of your psoriasis.
Recognizing the warning signs of psoriasis is vital for early intervention and effective management. Understanding the types, causes, and treatment options empowers individuals to take control of their condition and maintain a better quality of life. If you suspect you have psoriasis, don’t hesitate to seek medical advice to begin appropriate treatment promptly.
Note: This information is intended for educational purposes and should not replace professional medical advice. Always consult with a healthcare provider for personalized guidance.